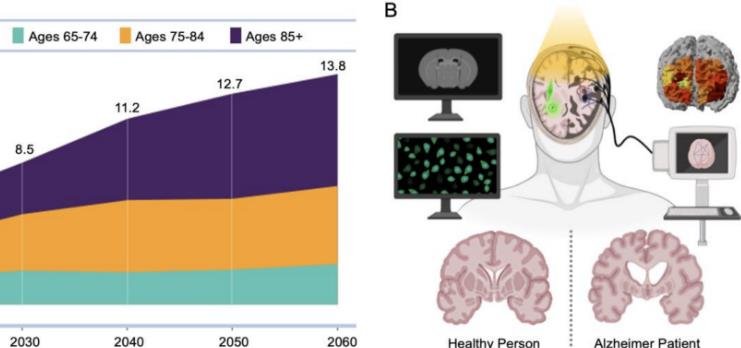
A new study published in Molecular Psychiatry has reviewed the use of neuroimaging techniques in the early and differential diagnosis of dementia, a leading cause of disability and death worldwide. The study highlights the contribution of structural and molecular imaging to a better understanding of the pathophysiology of neurodegenerative dementias and their clinical management.
What is dementia and why is it important to diagnose it early?
Dementia is a term that describes a group of symptoms affecting memory, thinking, behaviour and daily functioning. There are many types of dementia, such as Alzheimer’s disease (AD), Lewy Body dementia (LBD), vascular dementia (VaD) and Frontotemporal dementia (FTD). Each type of dementia has a different underlying cause and pattern of brain damage.
Early and accurate diagnosis of dementia subtype is critical for several reasons:
- It can help exclude reversible causes of memory problems, such as infections, vitamin deficiencies, medication side effects or depression.
- It can help optimise clinical care, such as providing appropriate medication, counselling, support and palliative care.
- It can help offer opportunities for secondary prevention, such as managing cardiovascular risk factors, lifestyle interventions or cognitive stimulation.
- It can help increase prognostic accuracy, such as estimating the rate of progression, the risk of complications or the need for long-term care.
- It can help identify the right people to benefit from disease modifying therapies, once these become available.
How can neuroimaging techniques help diagnose dementia?
Neuroimaging techniques are methods that allow visualising the structure and function of the brain. They can provide information about the location, extent and nature of brain damage in people with dementia. They can also reveal biomarkers that indicate the presence and severity of pathological processes in the brain, such as inflammation, amyloid plaques, tau tangles or synaptic loss.
The study reviewed the use of two main types of neuroimaging techniques: magnetic resonance imaging (MRI) and positron emission tomography (PET).
MRI
MRI is a technique that uses magnetic fields and radio waves to create detailed images of the brain. MRI can show structural changes in the brain, such as atrophy (shrinkage), white matter lesions (damage to the nerve fibres) or microbleeds (small areas of bleeding).
Structural MRI is widely used in clinical practice and can help exclude reversible causes of memory problems. However, it has relatively low sensitivity for the early and differential diagnosis of dementia subtypes. This is because structural changes in the brain often occur late in the disease course and overlap among different types of dementia.
Multimodal MRI is a technique that combines different MRI methods to measure different aspects of brain function, such as blood flow, metabolism, connectivity or network activity. Multimodal MRI can provide more information about the functional status of the brain and may improve the early and differential diagnosis of dementia subtypes. For example, multimodal MRI can help distinguish AD from FTD by showing different patterns of hypoperfusion (reduced blood flow) or hypometabolism (reduced energy use) in specific brain regions.
PET
PET is a technique that uses radioactive tracers to measure molecular processes in the brain. PET can show molecular changes in the brain, such as glucose metabolism, amyloid deposition, tau accumulation or synaptic density.
18F-fluorodeoxyglucose PET (FDG-PET) is a technique that measures glucose metabolism in the brain. Glucose is the main source of energy for brain cells and reflects their activity. FDG-PET can show areas of reduced glucose metabolism in the brain, indicating impaired function. FDG-PET has high sensitivity and specificity for AD and FTD. For example, FDG-PET can help differentiate AD from FTD by showing reduced glucose metabolism in the posterior cingulate cortex (a region involved in memory) in AD and in the frontal lobes (regions involved in behaviour) in FTD.
Amyloid PET is a technique that uses tracers that bind to amyloid plaques in the brain. Amyloid plaques are abnormal deposits of protein fragments that accumulate outside brain cells and are a hallmark of AD. Amyloid PET can show areas of increased amyloid deposition in the brain, indicating AD pathology. Amyloid PET can improve the differential diagnosis of AD and non-AD dementias. For example, amyloid PET can help rule out AD in cases of LBD or VaD by showing normal amyloid levels in these conditions.
Tau PET is a technique that uses tracers that bind to tau tangles in the brain. Tau tangles are abnormal deposits of protein filaments that accumulate inside brain cells and are another hallmark of AD. Tau PET can show areas of increased tau accumulation in the brain, indicating AD pathology. Tau PET can also improve the differential diagnosis of AD and non-AD dementias. For example, tau PET can help distinguish AD from FTD by showing different patterns of tau distribution in the brain, such as more widespread in AD and more focal in FTD.
Synaptic PET is a technique that uses tracers that bind to synaptic vesicle glycoprotein 2A (SV2A) in the brain. SV2A is a protein that is involved in synaptic transmission, the process of communication between brain cells. Synaptic PET can show areas of reduced synaptic density in the brain, indicating synaptic loss. Synaptic loss is a common feature of neurodegenerative dementias and correlates with cognitive impairment. Synaptic PET may be a sensitive early marker of dementia. For example, synaptic PET can help detect synaptic loss in the hippocampus (a region involved in memory) in prodromal AD, before amyloid or tau pathology is evident.
What are the limitations and future directions of neuroimaging techniques for dementia diagnosis?
Neuroimaging techniques have advanced our knowledge of the pathophysiology of neurodegenerative dementias and are increasingly being adopted into clinical practice for early and accurate diagnosis. However, there are still some limitations and challenges that need to be addressed:
- Neuroimaging techniques are expensive, invasive and not widely available in many settings.
- Neuroimaging techniques require standardisation, validation and harmonisation across different platforms, protocols and centres.
- Neuroimaging techniques need to be interpreted in the context of clinical history, examination and other biomarkers, such as cerebrospinal fluid analysis or genetic testing.
- Neuroimaging techniques need to account for individual variability, such as age, sex, ethnicity, education or comorbidities.
- Neuroimaging techniques need to be integrated into diagnostic criteria, guidelines and algorithms for dementia.
- Neuroimaging techniques need to be evaluated for their cost-effectiveness, impact on patient outcomes and ethical implications.
